
Psychedelics can treat emotional pain, but what about physical pain?
This article originally appeared on Cannabis.net and has been republished with permission.
Psychedelic drugs have not only made headlines in culture, but more recently in the medical community as well. “Classic” psychedelics such as psilocybin, LSD, DMT, and mescaline have attracted the attention of physicians for their ability to effectively and safely treat a range of conditions that even traditional psychedelics have struggled to treat successfully: depression, anxiety, and trauma.
There are dozens of studies, and counting, pointing to the effectiveness of various psychedelics in treating mental disorders. But what about physical pain?
Few but promising studies
This field of science is by no means new: one of the first studies to examine the pain-treating ability of psychedelics dates back to 1938, when Austrian-born physician Eric Kast fled the Nazis and settled in the United States. He took a job as an anesthesiologist at Cook County Hospital in Chicago. Kast was keen to learn about measuring pain responses and in 1962 developed the mechanical pain-inducing device, a device that subjects could use to inflict pain on themselves.
Two years later, he was drawn to the properties of LSD, which he administered to 50 pain patients. Her pain was caused by a variety of medical conditions ranging from gangrene to cancer. They were given synthetic opioids, but later in the study they were given 100 micrograms of LSD, which is an extremely high dose by any standards. “Compared to LSD-25, both [other] Medicines failed to have an analgesic effect,” he wrote in 1964.
Unfortunately, his studies were not expanded, but it was an outstanding study for a time.
Photo by Merlin Lightpainting by Pexels
Compared to studies on mental illness, there are very few studies examining how psychedelics can affect physical pain. However, the ones that are there certainly show promise.
chronic pain
A study by researchers at Imperial College London evaluated 11 participants who reported self-medication with psychedelic drugs. There was wide variation in doses, types of substances taken, frequency of use, and duration of effects, although the psychedelics most commonly used by participants were psilocybin mushrooms, while others took ketamine.
RELATED: Do Psychedelics Help Treat Pain?
Respondents were asked to participate in a one-hour discussion about their chronic pain and the effects of psychedelics on it. The results of the discussion were then analyzed by researchers, who found that pain scores decreased dramatically during and after psychedelics use. Positive feedback from participants varied: 7 said they had more control over their pain and life, 8 felt more compassionate about themselves and others, 4 said they were more motivated to take care of themselves, and all said the Experience changed her perspective and relationships with pain.
It was found that general acceptance of their situation, as well as freedom of choice and self-confidence, helped to improve overall pain management and well-being.
migraine
Another study showed surprising results on the effects of psilocybin on migraines. People who used psilocybin reported fewer migraines than those who received a placebo during the trial period. “This exploratory study suggests that there is a sustained therapeutic effect in migraines after a single administration of psilocybin,” the study states.
co-morbidities
In some studies, there appears to be a link between emotional and physical pain. More often than not, when psilocybin is able to treat an emotional symptom, it also improves a physical symptom—usually pain.
“If you look at the depression and PTSD studies, you can see how psychedelics could help people transform their relationship with their chronic pain,” says James Close, a PhD student at Imperial College London. “There is pre-clinical data that indicates the beneficial effect on the associated psychological mechanisms and neural pathways. The areas of pain, anxiety and depression are all interconnected. If you treat one, the other often gets better,” he said in a Sofia Phillips Thread article.
RELATED: Are Psychedelics Going Mainstream? Here’s how many Americans have tried psychedelics
Close believes there is a connection between persistent physical pain and ingrained habits in the brain. Hallucinogens may be able to promote brain plasticity, allowing the brain to start over.
Meanwhile, there are other studies that suggest that psychedelics’ ability to promote neuroplasticity in the brain may help us become less aware of pain by forming new brain connections. It also creates new pathways in the brain that change how we perceive pain.
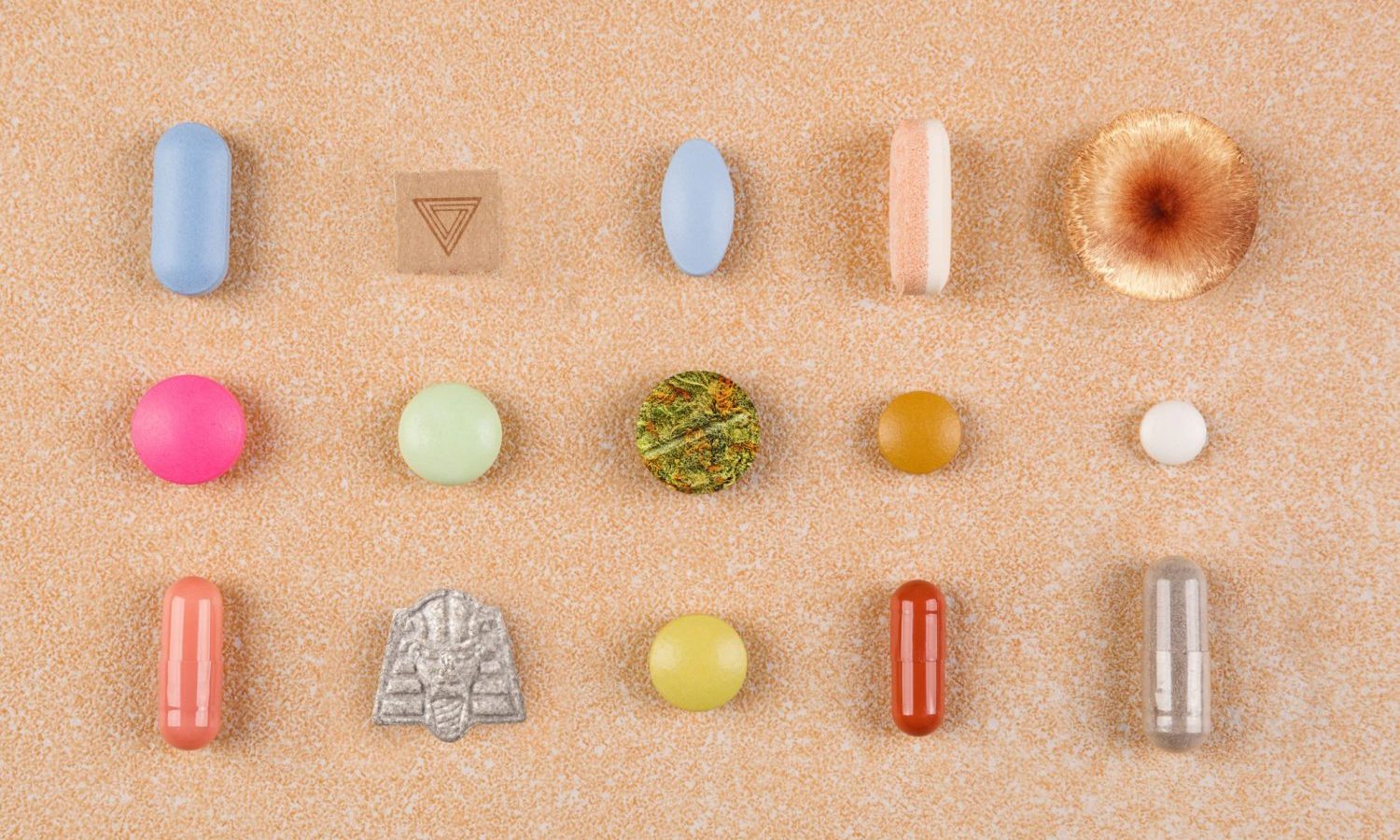 Photo by eskymaks/Getty Images
Photo by eskymaks/Getty Images
Companies expressing interest in psychedelics
The limited research we have has sparked interest from life science companies to delve deeper into the science of how psychedelics affect our perception and experience of pain. To date, there are some notable companies in this space, such as Tryp Therapeutics, which last year announced plans to conduct a Phase 2A clinical trial at the University of Michigan Medical School’s Chronic Pain & Fatigue Research Center. The study will evaluate the effects of TRYP-8802, an oral formulation of synthetic psilocybin, given to patients with psychotherapy to treat fibromyalgia.
The science is still in its infancy, but it seems that we can expect significant results in the near future. More importantly, it gives pain sufferers of all stripes a new kind of hope: that maybe someday they won’t have to rely on medication as a band-aid for pain, but that psychedelics, along with psychedelics therapy, can rewire and reset the brain to our relationship to change pain as a whole.

Post a comment: